Pivots on c2 lacks a body – Pivots on C2, a crucial anatomical structure in our cervical spine, may lack a physical body, but their functional significance is undeniable. Understanding the anatomy, biomechanics, and clinical implications of pivots on C2 is essential for healthcare professionals involved in the diagnosis and management of cervical spine disorders.
These unique joints, located at the juncture of the first and second cervical vertebrae, play a pivotal role in the intricate movements of our head and neck. Their dysfunction can lead to a range of clinical conditions, from atlantoaxial instability to occipital neuralgia.
This article delves into the multifaceted aspects of pivots on C2, exploring their anatomy, function, clinical significance, and management.
Pivots on C2
Pivots on C2, also known as atlantoaxial joints, are specialized synovial joints that connect the first and second cervical vertebrae (C1 and C2). These joints facilitate a unique range of motion, allowing for head rotation.
Anatomical Structure
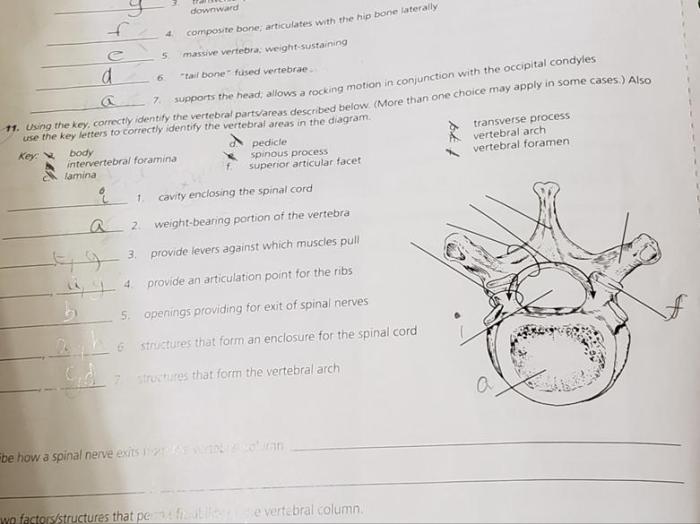
The pivots on C2 consist of the following anatomical components:
-
-*Dens of Axis (Odontoid Process)
A bony projection extending upward from the body of C2.
-*Atlas Ring
A ring-shaped structure that surrounds the dens of axis.
-*Transverse Ligament
Understanding the concept of pivots on c2 lacks a body is crucial for proper wound care. A comprehensive resource like the wound care ati post test can provide valuable insights into this topic. By delving deeper into pivots on c2 lacks a body, healthcare professionals can enhance their wound care skills and ensure optimal patient outcomes.
A strong ligament that attaches to the dens of axis and the inner surface of the atlas ring, stabilizing the joint.
Clinical Significance of Pivots on C2

Pivots on C2 are clinically significant because they can indicate underlying medical conditions. One such condition is atlantoaxial instability, which involves abnormal movement between the first and second cervical vertebrae (C1 and C2). This instability can lead to spinal cord compression and neurological symptoms.
Diagnostic Techniques
Diagnosing pivots on C2 involves a combination of imaging techniques and physical examination. Imaging techniques, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), can visualize the bony structures and soft tissues of the cervical spine. Physical examination can assess range of motion, tenderness, and neurological function.
Management of Pivots on C2
The management of pivots on C2 depends on the severity of the condition and the underlying cause. Conservative measures, such as physical therapy and rehabilitation, are often the first line of treatment. In some cases, surgical intervention may be necessary to stabilize the cervical spine and prevent further damage.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play a crucial role in managing pivots on C 2. These interventions aim to improve range of motion, strengthen the neck muscles, and reduce pain. Specific exercises and techniques may include:
- Range-of-motion exercises to increase flexibility and prevent stiffness
- Strengthening exercises to improve muscle stability and support
- Proprioceptive exercises to enhance balance and coordination
- Manual therapy techniques, such as massage and joint mobilization, to relieve pain and improve function
Surgical Intervention
Surgical intervention may be considered if conservative measures fail to alleviate symptoms or prevent further damage to the cervical spine. Surgical options include:
- Anterior cervical discectomy and fusion (ACDF): Removal of the herniated disc and fusion of the affected vertebrae to stabilize the spine
- Posterior cervical laminectomy: Removal of the lamina (a portion of the vertebra) to create more space for the spinal cord and nerves
- Cervical spinal cord stimulator: Implantation of a device that sends electrical impulses to the spinal cord to reduce pain
The choice of surgical intervention depends on the specific condition and the patient’s individual needs.
Differential Diagnosis of Pivots on C2
Pivots on C2, characterized by sudden, involuntary head movements due to a cervical spine abnormality, can sometimes resemble other conditions with similar symptoms. These conditions may share certain clinical features, but careful evaluation and differentiation are crucial for accurate diagnosis and appropriate management.
To establish a differential diagnosis, healthcare professionals consider other conditions that may mimic pivots on C 2. These include:
Occipital Neuralgia
- A condition involving the occipital nerve, which transmits sensory information from the upper neck and back of the head.
- Symptoms: Severe, sharp, stabbing, or burning pain in the back of the head, neck, or behind the eyes; may worsen with neck movement or pressure on the nerve.
- Diagnostic criteria: Nerve block injections that relieve pain can confirm the diagnosis.
Temporomandibular Joint Disorders (TMJ)
- Conditions affecting the temporomandibular joint (TMJ), which connects the jawbone to the skull.
- Symptoms: Pain in the jaw, face, or ears; clicking or popping sounds when opening or closing the mouth; difficulty chewing or biting; headaches.
- Diagnostic criteria: Physical examination, imaging studies (e.g., X-rays, MRI), and evaluation of jaw movement.
Advanced Imaging Techniques for Pivots on C2: Pivots On C2 Lacks A Body

Advanced imaging techniques play a crucial role in evaluating pivots on C2, providing detailed anatomical information that aids in diagnosis and treatment planning. Two commonly used techniques are MRI and CT scans.
Magnetic Resonance Imaging (MRI)
MRI utilizes strong magnetic fields and radio waves to generate detailed images of the spinal cord and surrounding structures. It excels in visualizing soft tissues, making it ideal for assessing ligamentous injuries, nerve root impingement, and spinal cord compression associated with pivots on C2.
However, MRI can be expensive and time-consuming, and it may not be readily available in all settings.
Computed Tomography (CT) Scan, Pivots on c2 lacks a body
CT scans use X-rays and computer processing to create cross-sectional images of the spine. They provide excellent visualization of bony structures, including the vertebrae, facet joints, and transverse ligament. CT scans are relatively quick and widely available, making them a valuable tool for evaluating bony abnormalities and fractures associated with pivots on C2.
However, CT scans offer limited soft tissue visualization compared to MRI.
Pivots on C2 in Sports and Physical Activities

Pivots on C2 are vulnerable to injury during sports and physical activities that involve sudden and forceful neck movements. Understanding the impact of these injuries is crucial for athletes, coaches, and healthcare professionals.
High-Risk Sports and Activities
Activities that increase the risk of pivots on C2 injuries include:
- Contact sports: Football, rugby, hockey
- Martial arts: Judo, wrestling, boxing
- Gymnastics: Vaulting, tumbling
- Diving: Springboard, platform
- High-impact activities: Running, jumping, falling
In these activities, the neck is subjected to excessive force, leading to potential ligamentous damage or dislocation.
Key Questions Answered
What are pivots on C2?
Pivots on C2 are unique joints located between the first and second cervical vertebrae, allowing for rotational movements of the head.
What clinical conditions involve pivots on C2?
Dysfunction of pivots on C2 can lead to conditions such as atlantoaxial instability, occipital neuralgia, and temporomandibular joint disorders.
How are pivots on C2 diagnosed?
Diagnosis involves a combination of physical examination, imaging techniques like X-rays, CT scans, and MRI.
What treatment options are available for pivots on C2?
Treatment options range from conservative measures like physical therapy to surgical interventions in severe cases.